Cancer type
WHAT IS CERVIX CANCER
Cervix cancer, also called cervical cancer, is a type of cancer that starts in the cells of the cervix. The cervix is the lower, narrow part of the uterus that connects to the vagina. This cancer usually develops slowly and is often caused by a long-lasting infection with certain types of the human papillomavirus (HPV). Regular screening tests, like Pap smears, can help detect it early when it’s easier to treat.
TYPES OF CERVIX CANCER
Cervical cancer is classified into two main types based on the kind of cells in which it starts. These types are important because they determine how the cancer behaves and is treated.
Squamous Cell Carcinoma
- What it is: This type begins in the thin, flat cells (squamous cells) lining the outer part of the cervix that connects to the vagina.
- How common: It is the most common type of cervical cancer, accounting for about 70-90% of cases.
- Risk factors: Closely linked to human papillomavirus (HPV) infection.
Adenocarcinoma
- What it is: This type starts in the glandular cells inside the cervical canal that produce mucus.
- How common: It is less common, making up about 10-20% of cervical cancers.
- Unique features: May be harder to detect with Pap smears because it occurs higher up in the cervix.
Other Rare Types
- Adenosquamous Carcinoma:
- A mix of squamous cells and glandular cells.
- Rare but more aggressive than the other two main types.
- Small Cell Neuroendocrine Carcinoma:
- A very rare and aggressive form of cervical cancer.
- Clear Cell and Other Rare Subtypes:
- Rare forms with distinct cellular features and behaviors.
Key Points
The type of cervical cancer is important for deciding treatment and predicting outcomes. Regular screening, HPV vaccination, and early diagnosis are key to managing and preventing most types of cervical cancer.
Causes of Cervix Cancer
Cervical cancer happens when the cells in the cervix (the lower part of the uterus) grow abnormally and uncontrollably. The main cause is long-term infection with certain types of the human papillomavirus (HPV), a common virus passed through sexual contact. Not everyone with HPV gets cervical cancer, but it increases the risk significantly.
Risk Factors for Cervical Cancer
Certain factors can raise the chances of developing cervical cancer:
- HPV Infection:
- The most important risk factor. Some types of HPV (like HPV 16 and 18) are more likely to cause cervical cancer.
- Weakened Immune System:
- A weak immune system (from HIV, organ transplants, or certain medications) makes it harder for the body to fight off HPV infections.
- Smoking:
- Chemicals in tobacco can damage cervical cells and increase the risk.
- Multiple Sexual Partners:
- Having many partners raises the chances of being exposed to HPV.
- Early Sexual Activity:
- Having sex at a young age can increase the risk of HPV infection.
- Long-Term Use of Birth Control Pills:
- Using oral contraceptives for more than 5 years may slightly increase the risk.
- Not Getting Regular Screenings:
- Pap smears and HPV tests can catch abnormal cells early before they turn into cancer.
- Family History:
- Having close relatives with cervical cancer may increase the risk.
- Pregnancies:
- Having many full-term pregnancies slightly raises the risk, possibly due to hormonal changes or exposure to HPV during pregnancy.
Key Point
Most cases of cervical cancer can be prevented by getting the HPV vaccine, practicing safe sex, and attending regular screening tests like Pap smear
TREATMENT
Treatment for Cervical Cancer
The treatment for cervical cancer depends on the stage of the cancer, the patient’s overall health, and whether they want to have children in the future. Here are the common treatment options:
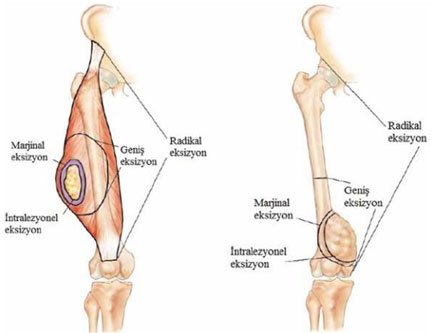
Surgery
- What it does: Removes the cancerous tissue.
- Types:
- Cone Biopsy: Removes only a small part of the cervix. Used for very early-stage cancer.
- Hysterectomy: Removes the entire uterus and cervix. This is common for early-stage cancer.
- Radical Hysterectomy: Removes the uterus, cervix, nearby tissues, and part of the vagina. Used for more advanced cases.
- Lymph Node Removal: Checks if cancer has spread to nearby lymph nodes.
Radiation Therapy
- What it does: Uses high-energy X-rays to kill cancer cells.
- How it’s done:
- External Radiation: A machine directs radiation to the cervix area.
- Internal Radiation (Brachytherapy): A small device with radiation is placed inside the cervix or vagina.
Chemotherapy
- What it does: Uses drugs to kill cancer cells or stop them from growing.
- When it’s used:
- Often combined with radiation for advanced-stage cancer.
- Given through an IV or as pills in cycles.
Targeted Therapy
- What it does: Focuses on specific changes in cancer cells to stop their growth.
- Example: Bevacizumab (Avastin), a drug that stops cancer from growing new blood vessels.
Immunotherapy
- What it does: Helps the immune system fight cancer.
- Example: Drugs like pembrolizumab (Keytruda) are used for advanced cervical cancer with certain genetic markers.
Palliative Care
- What it does: Focuses on managing symptoms and improving quality of life, especially in advanced stages.
- Includes pain relief, emotional support, and other comfort measures.
What to Expect
- Early-stage cancer often requires only surgery or radiation.
- Advanced cancer may need a combination of chemotherapy, radiation, and other therapies.
- Follow-up care is essential to monitor for recurrence.
Key Tip: Regular Pap smears and HPV vaccinations can help prevent cervical cancer or catch it early when it’s easier to treat.
PREVENTION
How to Prevent Cervical Cancer
Cervical cancer can often be prevented with healthy habits, vaccinations, and regular check-ups. Here are some simple ways to reduce the risk:
Get the HPV Vaccine
- The HPV vaccine protects against the types of HPV that cause most cases of cervical cancer.
- It’s best to get vaccinated between ages 9 and 26, but adults up to age 45 may also benefit.
Go for Regular Screenings
- Regular Pap smears and HPV tests can find abnormal cells in the cervix early, before they turn into cancer.
- Women should start screening at age 21 and follow their doctor’s advice about how often to test.
Practice Safe Sex
- Using condoms or other protection can lower the risk of HPV and other sexually transmitted infections.
- Limit the number of sexual partners to reduce the chance of exposure to HPV.
Quit Smoking
- Smoking damages the cells of the cervix and makes it harder for the body to fight HPV infections.
- Quitting smoking can lower your risk.
Take Care of Your Health
- Keep your immune system strong by eating healthy, staying active, and managing stress.
- If you have conditions like HIV, work with your doctor to control them, as they can increase your risk.
Use Birth Control Safely
- Long-term use of birth control pills slightly increases the risk of cervical cancer. Talk to your doctor about the best options for you.
Key Tip
Prevention starts with the HPV vaccine and regular check-ups. If you notice any unusual symptoms, like bleeding or pain, visit your doctor right away. Early action can save lives!
NEWER ADVANCEMENTS AND RESEARCH
Recent advancements in cervical cancer research have led to significant improvements in prevention, detection, and treatment. Here are some key developments:
Enhanced Screening Methods
- At-Home HPV Tests: The FDA has approved the first at-home HPV self-collection tests, allowing women to collect samples privately and send them to a lab for analysis. This innovation aims to increase screening rates, especially among those who may avoid traditional exams.
- AI-Assisted Diagnosis: Artificial intelligence is being utilized to analyze cervical cytology images, improving the accuracy and efficiency of detecting precancerous changes. This technology assists pathologists in identifying abnormalities more effectively.
Vaccination Progress
- HPV Vaccination: The HPV vaccine, initially aimed at preventing cervical cancer in women, has also been shown to reduce cancer risks in men, including cancers of the mouth and throat. This underscores the importance of vaccinating both boys and girls to lower future cancer risks.
Treatment Innovations
- New Chemotherapy Regimen: A recent clinical trial demonstrated that administering a short course of chemotherapy before the standard chemoradiation treatment can reduce the risk of death by 40% and decrease cancer recurrence by 35%. This approach is considered the most significant advancement in cervical cancer treatment in over two decades.
- Immunotherapy: Drugs like pembrolizumab (Keytruda) have been approved for treating advanced cervical cancer, offering new options for patients with recurrent or metastatic disease. These therapies work by enhancing the body’s immune response to target cancer cells.
- Antibody-Drug Conjugates: Tivdak (tisotumab vedotin) is a newly approved treatment for recurrent or metastatic cervical cancer. It combines an antibody with a chemotherapy drug to specifically target and kill cancer cells, providing a new option for patients whose cancer
These advancements represent significant progress in the fight against cervical cancer, offering hope for better prevention, earlier detection, and more effective treatments.
