Cancer type
WHAT IS ENDOMETRIUM CANCER
Endometrial cancer is a type of cancer that originates in the endometrium, the lining of the uterus. It is the most common type of uterine cancer and typically develops in the cells that form the inner layer of the uterine wall.
Key Characteristics:
- Cause: While the exact cause is not always clear, factors such as hormonal imbalances, particularly excess estrogen, play a significant role.
- Symptoms: Common symptoms include abnormal vaginal bleeding (especially after menopause), pelvic pain, and changes in menstruation.
- Risk Factors: Obesity, age (common in postmenopausal women), diabetes, polycystic ovary syndrome (PCOS), a history of irregular ovulation, and the use of estrogen therapy without progesterone can increase the risk.
- Diagnosis: Diagnosis is often made through procedures like an endometrial biopsy, transvaginal ultrasound, or hysteroscopy.
- Treatment: Depending on the stage and spread, treatment options may include surgery (hysterectomy), radiation therapy, chemotherapy, hormone therapy, or a combination of these.
Early detection of endometrial cancer often leads to effective treatment and a high survival rate, as it frequently causes noticeable symptoms in its early stages.
TYPES OF ENDOMETRIUM CANCER
Endometrial cancer is classified into two main types based on the cells from which the cancer originates and their behavior. These are Type 1 and Type 2 endometrial cancer, with further subtypes under each.
Type 1 Endometrial Cancer (Estrogen-Dependent)
Characteristics:
- Often linked to excess estrogen.
- Generally has a favorable prognosis.
- Grows slowly and is detected early due to symptoms like abnormal bleeding.
Subtype:
Endometrioid Adenocarcinoma:- The most common type, making up approximately 75-80% of cases.
- Tumor cells resemble the normal endometrial lining.
- Often associated with conditions like obesity, polycystic ovary syndrome (PCOS), and estrogen therapy.
Type 2 Endometrial Cancer (Non-Estrogen-Dependent)
- Characteristics:
- Not related to estrogen exposure.
- More aggressive with a higher risk of metastasis.
- Often diagnosed at an advanced stage.
Subtypes:
- Serous Carcinoma:
- Aggressive and accounts for about 10% of endometrial cancers.
- More common in older women and often not related to hormonal risk factors.
- Clear Cell Carcinoma:
- Rare and highly aggressive.
- Typically associated with a poor prognosis.
- Carcinosarcoma (Malignant Mixed Mullerian Tumor):
- Contains both carcinoma (epithelial) and sarcoma (connective tissue) components.
- Aggressive with a high risk of recurrence and metastasis.
- Serous Carcinoma:
Other Variants:
- Undifferentiated/Anaplastic Carcinoma:
- Rare, with poorly differentiated cells.
- Extremely aggressive and has a poor prognosis.
- Neuroendocrine Tumors:
- Rare, involving neuroendocrine cells.
- Includes small cell and large cell neuroendocrine carcinoma.
Clinical Importance:
- The classification affects treatment decisions and prognosis:
- Type 1 cancers generally respond well to surgery and hormone therapy.
- Type 2 cancers often require more aggressive treatment, including chemotherapy and radiation therapy.
Proper histological diagnosis and staging are critical for determining the appropriate course of treatment.
Causes of Endometrial Cancer
Endometrial cancer happens when the cells in the lining of the uterus (the endometrium) grow out of control. The exact cause isn’t always known, but it is often linked to hormonal imbalances, especially when there is too much estrogen compared to another hormone called progesterone. This imbalance can make the lining of the uterus grow too thick, increasing the risk of cancer.
CAUSES AND RISK FACTORS OF ENDOMETRIUM CANCER
Risk Factors for Endometrial Cancer
Certain things can make it more likely for someone to develop endometrial cancer. These include:
Age:
Most cases happen in women over 50, especially after menopause.
Hormonal Imbalance:
High levels of estrogen without enough progesterone can increase risk.
This can happen with hormone therapy (if progesterone isn’t included) or certain medical conditions.
Obesity:
Extra fat in the body can produce estrogen, which increases the risk.
Diabetes:
Having diabetes may raise the chance of getting endometrial cancer.
Irregular Ovulation:
Conditions like polycystic ovary syndrome (PCOS) or not having regular periods can cause hormonal imbalance.
Never Being Pregnant:
Women who have never been pregnant have a higher risk because pregnancy changes hormone levels.
Early Periods or Late Menopause:
Starting periods at a young age or having menopause later means the endometrium is exposed to hormones for a longer time.
Family History:
A family history of endometrial or colorectal cancer may increase the risk, especially with genetic conditions like Lynch syndrome.
Tamoxifen Use:
This breast cancer drug slightly raises the risk of endometrial cancer.
Radiation Therapy:
Previous radiation to the pelvis can increase the risk of cancer in the uterus.
Causes
- Gene Changes (Mutations): Changes in the DNA of colon cells can make them grow out of control and form a tumor.
- Polyps: Small growths in the colon can sometimes turn into cancer if not removed.
- Family History: Certain inherited gene conditions, like Lynch syndrome, increase the chance of colon cancer.
Risk Factors
Things You Can’t Control:
- Age: Most people with colon cancer are over 50, but it can happen earlier.
- Family History: If close family members have had colon cancer, your risk is higher.
- Genetic Conditions:
- Inherited syndromes like Lynch syndrome or familial adenomatous polyposis (FAP).
- Medical History:
- Having inflammatory bowel diseases like Crohn’s or ulcerative colitis increases risk.
Things You Can Control:
- Diet:
- Eating lots of red or processed meats (like bacon or sausage) increases risk.
- A diet low in fiber, fruits, and vegetables can also contribute.
- Lack of Exercise: Being inactive can raise your risk.
- Obesity: Being very overweight increases the likelihood of developing colon cancer.
- Smoking: Tobacco use damages cells in the colon.
- Alcohol: Drinking too much alcohol regularly can increase your risk.
- Diabetes: People with poorly controlled diabetes are at a higher risk.
Key Point
While some of these factors, like age, can’t be changed, others, like maintaining a healthy weight or balancing hormones, may help reduce the risk. Always talk to a doctor if you’re concerned about your risk.
PREVENTION
Maintain a Healthy Weight
- Obesity is a major risk factor for endometrial cancer because excess fat increases estrogen levels.
- Eating a balanced diet and staying active can help maintain a healthy weight.
Be Physically Active
- Regular exercise helps control weight and may reduce hormone levels linked to cancer risk.
- Aim for at least 30 minutes of moderate physical activity most days of the week.
Manage Hormonal Balance
- If you’re using hormone replacement therapy (HRT) for menopause, talk to your doctor about using both estrogen and progesterone to balance hormone levels.
- Avoid long-term use of estrogen-only therapy unless medically necessary.
Treat and Manage Health Conditions
- Address conditions like polycystic ovary syndrome (PCOS) and diabetes, as they can increase risk.
- Controlling blood sugar levels and managing irregular periods can help.
Use Birth Control Pills (If Appropriate)
- Long-term use of birth control pills can lower the risk of endometrial cancer by regulating hormones.
- Discuss this option with your doctor, as it may not be suitable for everyone.
Be Aware of Family History
- If you have a family history of endometrial or colorectal cancer, especially linked to Lynch syndrome, consult a genetic counselor.
- Women with Lynch syndrome may benefit from regular screenings or preventative measures like a hysterectomy after childbearing.
Watch for Symptoms
- Early detection can prevent the cancer from progressing. Watch for symptoms like unusual vaginal bleeding and see a doctor immediately if they occur.
Avoid Smoking
- Smoking can contribute to many types of cancer, including endometrial cancer. Quitting smoking is beneficial for overall health.
Key Point
By adopting healthy habits, staying informed about risks, and consulting a healthcare provider about hormone therapies or family history, you can lower your chances of developing endometrial cancer.
TREATMENT
Treatment for endometrial cancer depends on the cancer’s type, stage, overall health, and individual preferences. The main goal of treatment is to remove or destroy cancer while preserving as much normal function as possible.
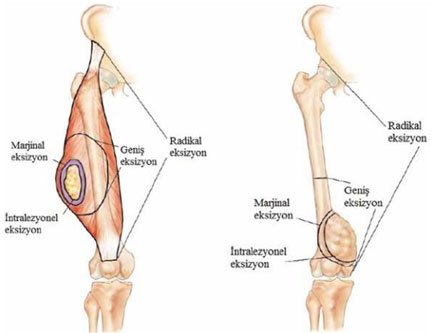
Surgery
Surgery is the most common treatment, especially in the early stages of endometrial cancer. It involves removing the cancerous tissue from the uterus.
- Hysterectomy: Removal of the uterus. In some cases, the ovaries and fallopian tubes (salpingo-oophorectomy) are also removed.
- Lymph Node Dissection: Nearby lymph nodes may be removed to check if the cancer has spread.
- Minimally Invasive Surgery: Such as laparoscopic or robotic surgery, may be used for quicker recovery.
Radiation Therapy
Radiation therapy uses high-energy beams to kill cancer cells. It can be used:
- Before surgery to shrink tumors.
- After surgery to destroy remaining cancer cells.
- As the main treatment if surgery isn’t an option.
Types of Radiation:
- External Beam Radiation Therapy (EBRT): Delivers radiation from outside the body.
- Brachytherapy: Places a radioactive source inside the vagina, targeting the cancer more precisely.
Hormone Therapy
Hormone therapy is used to slow the growth of cancer cells, especially in advanced or recurrent cases.
- Progestin Therapy: Uses synthetic progesterone to counteract estrogen-driven cancer growth.
- Aromatase Inhibitors: Reduce estrogen levels, particularly in postmenopausal women.
Immunotherapy
- Helps your immune system recognize and attack cancer cells.
- When It’s Used:
- Mostly for advanced colon cancer with specific genetic features.
Chemotherapy
Chemotherapy involves using drugs to kill cancer cells or stop their growth. It’s often used for:
- Advanced cancer that has spread beyond the uterus.
- Type 2 endometrial cancers, which are more aggressive.
- Recurrent cancer.
Chemotherapy drugs can be given orally or through an IV and are often used in combination.
Immunotherapy
For advanced or recurrent cases, immune checkpoint inhibitors can help the body’s immune system recognize and attack cancer cells. This is particularly helpful for cancers with certain genetic mutations (e.g., mismatch repair deficiency).
Targeted Therapy
Targeted drugs focus on specific changes in cancer cells. These therapies may be used for advanced endometrial cancer or in clinical trials.
Palliative Care
For advanced-stage cancer, palliative treatments focus on managing symptoms like pain or bleeding and improving the quality of life.
Treatment by Stage
- Early-Stage (Stage I): Surgery (hysterectomy) is usually enough; radiation or hormone therapy may be added if necessary.
- Intermediate-Stage (Stage II): Surgery followed by radiation or a combination of radiation and chemotherapy.
- Advanced-Stage (Stage III & IV): A combination of surgery, chemotherapy, radiation, and/or targeted therapy is often used.
Follow-Up Care
After treatment, regular follow-up appointments are essential to monitor for recurrence and manage any long-term side effects.
Note: The choice of treatment is highly individual, and decisions should be made in consultation with a healthcare provider.
NEWER ADVANCEMENTS AND RESEARCH
Recent advancements in endometrial cancer research have led to significant improvements in diagnosis and treatment, offering new hope for patients.
Immunotherapy Enhancements
Immunotherapy has become a pivotal component in treating advanced endometrial cancer. Notably, the U.S. Food and Drug Administration (FDA) approved several immune checkpoint inhibitors:
- Durvalumab (Imfinzi): Approved in June 2024 for use with chemotherapy in patients with advanced endometrial cancer exhibiting mismatch repair deficiency (dMMR). Clinical trials demonstrated that this combination reduced the risk of disease progression or death by 58% compared to chemotherapy alone.
- Pembrolizumab (Keytruda): Also approved in June 2024 for use alongside chemotherapy for primary advanced or recurrent endometrial carcinoma. Studies indicated a 40% reduction in disease progression or death in patients with mismatch repair proficient cancer and a 70% reduction in those with mismatch repair deficient cancer.
- Dostarlimab (Jemperli): Approved for treating recurrent or advanced endometrial cancer with dMMR. Clinical trials have shown promising results, leading to its approval in multiple regions.
Molecular Profiling and Targeted Therapies
Advancements in molecular profiling have enabled the identification of specific genetic mutations and biomarkers in endometrial cancer. This precision medicine approach allows for tailored treatments targeting these mutations, improving efficacy and reducing side effects.
Artificial Intelligence in Diagnosis
The integration of artificial intelligence (AI) in pathology has enhanced diagnostic accuracy. For instance, the development of AI models like EndoNet assists pathologists in classifying tumor grades without manual annotations, streamlining the diagnostic process.
Combination Therapies
Combining immunotherapy with traditional treatments such as chemotherapy and radiation has shown improved outcomes. Clinical trials are ongoing to determine the most effective combinations and sequences of these therapies.
Enhanced Screening and Early Detection
Research into more effective screening methods is underway, particularly for populations at higher risk. Studies have highlighted the need for improved diagnostic tools, especially for Black women, as common tests like transvaginal ultrasounds may miss cases in this demographic.
These advancements represent a significant shift towards more personalized and effective management of endometrial cancer, improving patient outcomes and quality of life.
