Cancer type
Definition of Ovarian cancer
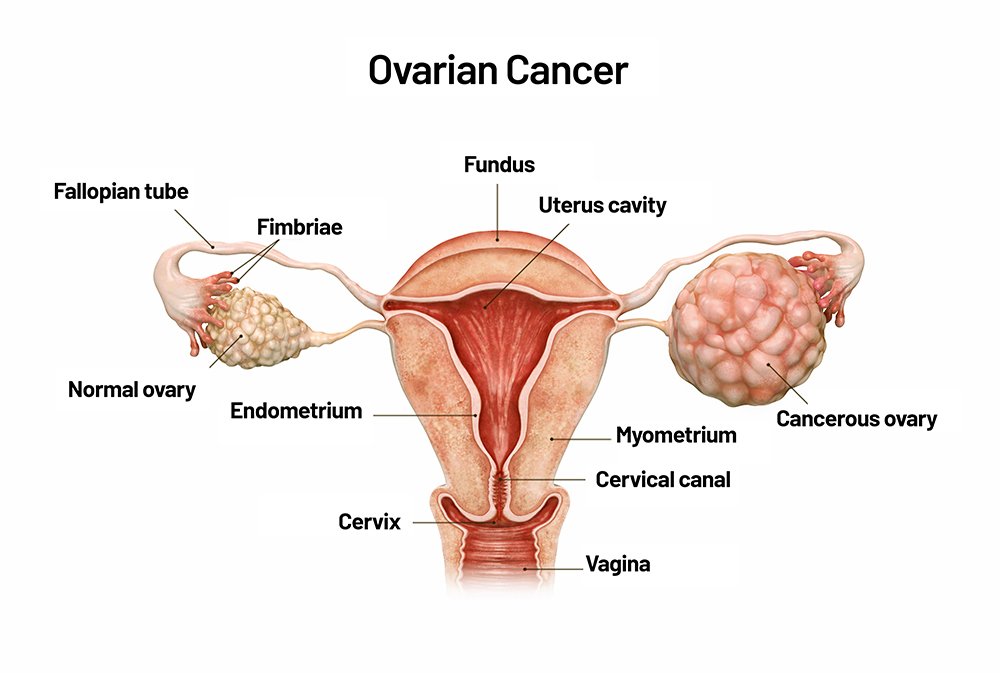
Ovarian cancer is a type of cancer that begins in the ovaries, which are the reproductive glands found in females responsible for producing eggs (ova) and hormones like estrogen and progesterone. This cancer develops when cells in the ovaries start to grow uncontrollably, forming a tumor. If untreated, ovarian cancer cells can spread to nearby tissues and other parts of the body, a process known as metastasis.
Ovarian cancer is often difficult to detect in its early stages because symptoms are typically mild and nonspecific. Symptoms can include abdominal bloating, pelvic pain, difficulty eating, and urinary frequency. Common types of ovarian cancer include epithelial ovarian cancer, which starts in the layer of cells covering the ovary, and less common types like germ cell tumors and stromal cell tumors. Treatment typically involves surgery and may also include chemotherapy or targeted therapy, depending on the stage and type of cancer.
TYPES OF OVARIAN CANCERS
Ovarian cancer is classified into several types based on the type of cells where the cancer begins. The main types of ovarian cancer include:
Epithelial Ovarian Cancer
- This is the most common type of ovarian cancer, accounting for about 90% of cases.
- It starts in the layer of cells (epithelium) covering the outer surface of the ovary.
- Subtypes of epithelial ovarian cancer include:
- Serous carcinoma (high-grade or low-grade)
- Mucinous carcinoma
- Endometrioid carcinoma
- Clear cell carcinoma
- High-grade serous carcinoma is the most common and aggressive subtype.
Germ Cell Ovarian Tumors
- These tumors originate in the cells that produce eggs (germ cells).
- They are rare, making up about 5-10% of ovarian cancers.
- Most germ cell tumors are benign, but some can be malignant.
- Types of malignant germ cell tumors include:
- Dysgerminomas
- Yolk sac tumors
- Choriocarcinomas
- Teratomas (immature teratomas are malignant, while mature teratomas are usually benign)
Stromal Cell Tumors
- These tumors start in the ovarian stroma, which produces hormones and connects the ovarian tissues.
- They are relatively rare, making up about 1-2% of ovarian cancers.
- Stromal cell tumors often secrete hormones like estrogen and progesterone.
- Types of stromal tumors include:
- Granulosa cell tumors (most common type of stromal tumor)
- Sertoli-Leydig cell tumors
Small Cell Carcinoma of the Ovary
- This is an extremely rare and aggressive form of ovarian cancer.
- It usually affects younger women.
- There are two main subtypes: hypercalcemic and pulmonary types.
Primary Peritoneal Cancer (PPC)
- Although not technically originating in the ovaries, PPC behaves similarly to epithelial ovarian cancer.
- It arises from the lining of the abdomen (peritoneum) and shares similar symptoms and treatment approaches with ovarian cancer.
Each type of ovarian cancer has distinct biological behaviors, and the treatment approach may vary depending on the type and stage of the cancer.
CAUSES AND RISK FACTORS OF OVARIAN CANCERS
The exact cause of ovarian cancer is not fully understood, but certain risk factors have been identified that can increase the likelihood of developing the disease. These risk factors, which may interact in complex ways, include genetic, hormonal, and lifestyle elements:
Genetic Factors
- Inherited gene mutations: The most significant risk factor for ovarian cancer is a family history of certain genetic mutations, particularly in the BRCA1 and BRCA2 genes. Women with these mutations have a much higher risk of ovarian and breast cancer.
- Family history of cancer: Having a close relative (such as a mother, sister, or daughter) with ovarian cancer or certain other cancers (like breast or colorectal cancer) can increase risk.
- Lynch syndrome: Also known as hereditary nonpolyposis colorectal cancer (HNPCC), Lynch syndrome is an inherited genetic mutation that raises the risk of several types of cancer, including ovarian.
Age
- Most cases of ovarian cancer are diagnosed in women over the age of 50, with the majority occurring in postmenopausal women. The risk increases with age, peaking in a woman’s late 70s.
Reproductive History and Infertility
- Never being pregnant: Women who have not had children may have a slightly higher risk of ovarian cancer.
- Late or no pregnancy: Women who have their first full-term pregnancy after age 35 or who have never carried a pregnancy to term may have an increased risk.
- Infertility: Certain infertility issues or prolonged use of fertility treatments (though research is ongoing) may raise ovarian cancer risk.
Hormone Replacement Therapy (HRT)
- Long-term use of hormone replacement therapy, particularly estrogen-only HRT, is associated with a higher risk of ovarian cancer. The risk seems to decrease after discontinuing HRT.
Endometriosis
- Women with endometriosis, a condition where tissue similar to the lining of the uterus grows outside the uterus, have a slightly increased risk of certain types of ovarian cancer.
Personal History of Certain Cancers
- A personal history of breast, uterine, or colorectal cancer can increase the risk of ovarian cancer, especially if linked to inherited genetic mutations.
Lifestyle Factors
- Obesity: Obesity has been linked to a slightly higher risk of developing ovarian cancer, especially in younger women.
- Smoking: Smoking is associated with an increased risk of certain types of ovarian cancer, particularly mucinous ovarian cancer.
Environmental Factors
- Some environmental exposures, such as asbestos, have been studied for links to ovarian cancer, though evidence is still limited.
Menstrual Factors
Early menstruation and late menopause: Women who began menstruating at an early age or went through menopause later in life may have a slightly increased risk, possibly due to the prolonged exposure to estrogen.
Protective Factors
- Oral contraceptive use: Birth control pills have been shown to lower the risk of ovarian cancer, with risk reduction increasing with longer use.
- Pregnancy and breastfeeding: Both have been associated with a reduced risk of ovarian cancer, possibly due to reduced ovulation cycles.
While these risk factors can increase the chances of developing ovarian cancer, having one or even several of these factors does not mean a woman will develop ovarian cancer. Conversely, some women develop ovarian cancer without any known risk factors.
PREVENTION OF OVARIAN CANCERS
While there is no guaranteed way to prevent ovarian cancer, certain strategies may help reduce the risk. These prevention methods focus on lifestyle modifications, medical options, and increased awareness of personal risk factors:
Use of Oral Contraceptives (Birth Control Pills)
- Long-term use of birth control pills has been shown to significantly reduce the risk of ovarian cancer. The protective effect increases with the length of use and can last for many years after stopping the pill.
- However, birth control pills may have risks of their own, so discussing with a healthcare provider is recommended to weigh the benefits and risks.
Pregnancy and Breastfeeding
- Women who have had full-term pregnancies, particularly before age 30, and those who breastfeed may have a reduced risk of ovarian cancer. The more pregnancies a woman has, the lower her risk may be.
Consideration of Surgery for High-Risk Individuals
- Risk-reducing surgery: Women with a very high risk of ovarian cancer due to genetic mutations, such as BRCA1, BRCA2, or Lynch syndrome, may consider preventive surgery (prophylactic oophorectomy) to remove the ovaries and fallopian tubes.
- Tubal ligation and hysterectomy: These procedures, typically done for other medical reasons, may also reduce ovarian cancer risk. Tubal ligation, or “tying the tubes,” has been linked to a lower risk, especially for certain types of ovarian cancer.
Genetic Testing and Counseling
- Women with a family history of ovarian, breast, or certain other cancers should consider genetic counseling. A genetic counselor can help assess the risk of inherited cancer syndromes and may recommend genetic testing.
- If certain gene mutations (e.g., BRCA1 or BRCA2) are detected, tailored prevention strategies can be considered.
Healthy Lifestyle Choices
- Maintain a healthy weight: Obesity has been associated with an increased risk of ovarian cancer, so regular physical activity and a balanced diet may reduce risk.
- Avoid smoking: Smoking is linked to a higher risk of certain ovarian cancer subtypes, such as mucinous carcinoma. Quitting smoking reduces the risk and improves overall health.
- Limit hormone replacement therapy (HRT): If HRT is needed for menopausal symptoms, it is advised to use the lowest dose for the shortest time possible, as prolonged use may increase ovarian cancer risk.
Regular Medical Check-Ups and Awareness of Symptoms
- Early detection can improve outcomes, so being attentive to potential symptoms (such as bloating, pelvic pain, or difficulty eating) and discussing any concerns with a healthcare provider can be beneficial.
- Women at higher risk may discuss with their doctor about more frequent monitoring, though current screening methods (like CA-125 blood tests or transvaginal ultrasound) are not recommended for routine screening in average-risk women due to limited effectiveness in early detection.
Awareness of Endometriosis Risk
- Women with endometriosis should be aware of their slightly increased risk of ovarian cancer. Managing endometriosis with medical guidance and discussing concerns with a healthcare provider may help tailor prevention and monitoring strategies.
While these methods do not guarantee prevention, they can reduce the risk of ovarian cancer, especially for those at higher risk. Regular discussions with healthcare providers about personal risk factors and options for risk reduction are important steps in managing and potentially lowering the risk of ovarian cancer.
TREATMENT FOR OVARIAN CANCER
The treatment for ovarian cancer depends on the type and stage of the cancer, as well as the patient’s overall health. Common treatments include surgery, chemotherapy, and sometimes targeted therapy or radiation. Here’s an overview:
Surgery
- Goal: To remove as much of the cancer as possible, which is called “debulking.”
- Types of Surgery: The type of surgery depends on how far the cancer has spread. This may include:
- Oophorectomy: Removal of one or both ovaries.
- Salpingo-oophorectomy: Removal of the ovaries and fallopian tubes.
- Hysterectomy: Removal of the uterus.
- Lymph Node Removal: In advanced cases, nearby lymph nodes may be removed.
- For early-stage cancer, surgery may be the only treatment needed.
Chemotherapy
- Goal: To kill cancer cells that may remain after surgery or shrink the tumor before surgery.
- How It’s Given: Usually through an IV, but sometimes directly into the abdomen (intraperitoneal chemotherapy).
- When It’s Used: Often after surgery to reduce the chance of the cancer returning, but can also be used before surgery (called neoadjuvant chemotherapy) if the tumor is large.
Targeted Therapy
- Goal: To target specific features of cancer cells, which can help kill them or stop their growth.
- Types:
- PARP inhibitors: Useful for patients with BRCA gene mutations or certain other genetic profiles.
- Bevacizumab (Avastin): A drug that stops blood flow to tumors.
- When It’s Used: Often used for women with advanced ovarian cancer or if the cancer returns after initial treatment.
Radiation Therapy
- Goal: To kill cancer cells using high-energy rays.
- When It’s Used: Rarely used as a main treatment for ovarian cancer, but sometimes used for specific cases, like treating small tumors in specific areas.
Hormone Therapy
- Goal: To block hormones that some types of ovarian cancer cells need to grow.
- When It’s Used: Mainly for certain rare types of ovarian cancer, such as stromal tumors.
Clinical Trials
- Goal: To offer access to new treatments not yet widely available.
- Why It’s Considered: Clinical trials may provide additional options, especially for advanced or recurrent ovarian cancer.
Supportive Care
- Goal: To help manage symptoms and side effects and improve quality of life.
- Options: Supportive care may include pain management, nutrition support, mental health counseling, and physical therapy.
Treatment Plan
Each patient’s treatment plan is personalized, often combining surgery and chemotherapy as the main treatments. Doctors may also recommend targeted therapy or other treatments based on the cancer’s stage and genetic profile. Regular follow-up is essential to monitor for any recurrence or new symptoms.
Newer Advancements/ Researches
Recent advancements in ovarian cancer research have led to promising developments in detection, treatment, and understanding of the disease. Key areas of progress include:
Targeted Therapies and Immunotherapy
- Antibody-Drug Conjugates (ADCs): These are engineered antibodies linked to chemotherapy drugs, designed to deliver treatment directly to cancer cells, minimizing damage to healthy tissue. The FDA’s approval of mirvetuximab soravtansine (Elahere) for platinum-resistant ovarian cancer exemplifies this approach.
- PARP Inhibitors: Drugs like niraparib have shown effectiveness, particularly in patients with BRCA mutations, by hindering cancer cells’ DNA repair mechanisms.
Immunotherapy: Research into vaccines aims to stimulate the immune system to recognize and attack ovarian cancer cells. For instance, Mayo Clinic is developing a vaccine to prevent tumor recurrence in advanced ovarian cancer patient
Early Detection and Screening
- Genetic Testing: Identifying mutations in genes like BRCA1 and BRCA2 helps assess risk and guide preventive measures. Advocacy for broader access to genetic screening is growing, emphasizing its role in early detection.
Biomarker Research: Efforts are underway to discover biomarkers that could lead to reliable screening tests, improving early detection rates.
Personalized Medicine
- Genomic Profiling: Analyzing the genetic makeup of tumors allows for treatments tailored to individual patients, enhancing effectiveness and reducing side effects. Studies have identified distinct genetic patterns in high-grade serous ovarian cancer, aiding in personalized treatment strategies.
Advanced Surgical Techniques
- Minimally Invasive Surgery: Laparoscopic and robotic-assisted surgeries offer less invasive options, leading to quicker recovery and fewer complications.
Artificial Intelligence (AI) and Machine Learning
- Predictive Analytics: AI models are being developed to predict treatment responses and survival outcomes, assisting in personalized treatment planning. For example, studies have shown AI’s potential in accurately predicting survival outcomes for ovarian cancer patients.
Nanotechnology
- Drug Delivery Systems: Nanoparticles are being explored to deliver chemotherapy directly to cancer cells, potentially increasing effectiveness and reducing side effects. Research indicates that nanotechnology can boost ovarian cancer immunotherapy by enhancing the delivery and efficacy of treatment
These advancements represent significant strides in the fight against ovarian cancer, offering hope for improved detection, more effective treatments, and better patient outcomes.
