Cancer type
Definition of Testicular cancer
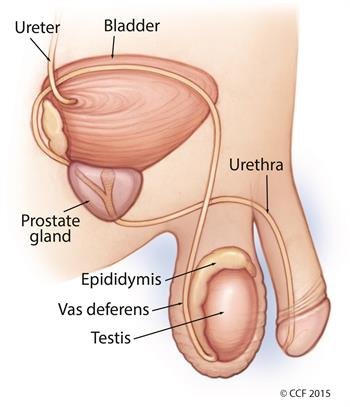
Testicular cancer is a type of cancer that starts in the testicles, which are the oval-shaped glands in men that produce sperm and testosterone (a male hormone). It happens when cells in the testicles grow abnormally and form a tumor. Testicular cancer is rare but usually treatable, especially if found early. It often affects younger men, typically between the ages of 15 and 35.
SYMPTOMS OF TESTICULAR CANCER
Symptoms of Testicular Cancer
The symptoms of testicular cancer can include:
Lump or swelling in the testicle:
- The most common sign is a painless lump or swelling in one testicle.
Change in size or shape of the testicle:
- One testicle may feel larger, firmer, or different than usual.
Feeling of heaviness in the scrotum:
- A sensation that the scrotum is heavier than normal.
Dull ache or pain:
- You may feel discomfort or pain in the lower belly, groin, or testicle.
Fluid buildup in the scrotum:
- Sudden collection of fluid around the testicle.
Back pain or chest discomfort (in advanced cases):
- This can happen if the cancer has spread to other parts of the body.
If you notice any of these symptoms, it’s important to see a doctor right away. Early detection makes treatment much easier and more effective.
Types of Testicular Cancer
Testicular cancer is classified based on the type of cells where it starts. The two main types are germ cell tumors and non-germ cell tumors:
Germ Cell Tumors:
These are the most common type, making up about 90-95% of testicular cancers. They start in the cells that produce sperm and are further divided into:
- Seminomas:
- Grow more slowly.
- Usually occur in men aged 25-45.
- Often respond well to treatment, even if they have spread.
- Non-seminomas:
- Grow and spread more quickly.
- Typically occur in younger men, usually in their late teens to early 30s.
- Includes subtypes like:
- Embryonal carcinoma.
- Yolk sac tumor.
- Choriocarcinoma.
- Teratoma.
Non-Germ Cell Tumors:
These are much rarer and include:
- Leydig Cell Tumors:
- Start in cells that make male hormones like testosterone.
- Usually grow slowly.
- Sertoli Cell Tumors:
- Begin in cells that support sperm production.
- Typically less aggressive.
Secondary Testicular Cancer:
This is when cancer spreads to the testicle from another part of the body, such as lymphoma, which is the most common type in older men.
Doctors use tests to determine the type of testicular cancer, which helps guide the best treatment approach. Most types respond well to treatment, especially when detected early.
CAUSES AND RISK FACTORS OF TESTICULAR CANCER
Causes of Testicular Cancer
The exact cause of testicular cancer isn’t always known, but it happens when healthy cells in the testicles start to grow uncontrollably and form a tumor. These changes are often linked to genetic or environmental factors, but specific triggers are not always clear.
Risk Factors for Testicular Cancer
Certain factors can increase the chance of developing testicular cancer, including:
Undescended Testicle (Cryptorchidism):
- If one or both testicles didn’t move into the scrotum before birth, the risk is higher, even if corrected later.
Family History:
- Having a father or brother with testicular cancer increases the risk.
Age:
- Testicular cancer is most common in young men, usually between the ages of 15 and 35.
Race/Ethnicity:
- White men have a higher risk compared to men of other races.
Abnormal Testicle Development:
- Conditions like Klinefelter syndrome, which affect testicle development, can increase the risk.
Personal History of Testicular Cancer:
- Men who have had cancer in one testicle are more likely to develop it in the other.
HIV Infection:
- Men with HIV, particularly those with AIDS, have a higher risk of testicular cancer.
Lifestyle Factors:
- While not well-understood, certain environmental exposures or toxins might increase the risk.
While these factors can increase the risk, having one or more of them doesn’t mean you’ll develop testicular cancer. Regular self-exams and early medical attention for changes can help with early detection and treatment.
TREATMENT OF TESTICULAR CANCER
Treatment of Testicular Cancer
Testicular cancer is highly treatable, especially when caught early. The treatment depends on the type of cancer, its stage, and your overall health. Here are the main treatment options:
Surgery:
- Orchiectomy (Removal of the testicle):
- The most common treatment for testicular cancer.
- The affected testicle is removed through a small incision in the groin.
- Lymph Node Surgery:
- If the cancer has spread, nearby lymph nodes in the abdomen may also be removed.
Radiation Therapy:
- Uses high-energy X-rays to kill cancer cells or stop them from growing.
- Often used for seminomas, which are more sensitive to radiation.
- Targets specific areas to minimize damage to healthy tissues.
Chemotherapy:
- Uses strong drugs to kill cancer cells or prevent them from spreading.
- Often recommended for non-seminomas or if the cancer has spread beyond the testicle.
- Can also be used after surgery to kill any remaining cancer cells.
Active Surveillance:
- For very early-stage cancer, your doctor may recommend monitoring with regular tests and scans instead of immediate treatment.
- This approach helps avoid unnecessary treatments while keeping a close watch on the cancer.
Stem Cell Transplant (Rare):
- Used in some advanced cases after high-dose chemotherapy.
- Healthy stem cells are used to rebuild the bone marrow after intensive treatment.
Reconstruction and Recovery:
- If desired, a prosthetic (artificial) testicle can be implanted for cosmetic purposes.
- Regular follow-ups are essential to monitor for recurrence or complications.
Testicular cancer has one of the highest cure rates, especially if treated early. Your doctor will recommend the best treatment based on your specific situation.
PREVENTION OF TESTICULAR CANCER
evention of Testicular Cancer
There’s no guaranteed way to prevent testicular cancer, but you can take steps to reduce your risk or detect it early:
Perform Regular Self-Exams:
- Check your testicles once a month for lumps, swelling, or changes in size or shape.
- Early detection is key, as testicular cancer is highly treatable when caught early.
Be Aware of Risk Factors:
- If you have a family history of testicular cancer or an undescended testicle, talk to your doctor about regular screenings.
Protect Your Testicles:
- Wear protective gear during sports or physical activities to avoid injuries to the testicles.
Maintain a Healthy Lifestyle:
- Eat a balanced diet, stay active, and avoid smoking or excessive alcohol consumption to improve overall health.
Treat Testicular Problems Early:
- Conditions like undescended testicles should be corrected early in life to reduce the risk.
While you can’t fully prevent testicular cancer, being proactive with self-exams and regular doctor visits can help detect it early when treatment is most effective.
NEWER ADVANCEMENTS/RESEARCHES IN TESTICULAR CANCER
Recent advancements in testicular cancer research have led to improved diagnostic methods and treatment options, offering hope for better patient outcomes.
Genetic Insights:
- Identification of New Gene Faults: Scientists have discovered new genetic mutations and evolutionary patterns that contribute to testicular cancer. These findings provide deeper insights into the disease’s development and potential treatment strategies.
Personalized Medicine:
- Molecular Profiling: Understanding the genetic makeup of a patient’s tumor allows for tailored treatments. For example, certain gene mutations found in testicular cancer cells have been linked to resistance to chemotherapy and predict poor outcomes. These findings may help personalize treatment and could also help find new drugs to treat testicular cancer.
Advances in Imaging and Surveillance:
- Safer Monitoring Techniques: After surgery for early-stage, low-risk testicular cancer, it’s safe to monitor for a recurrence using MRI scans or fewer CT scans than are currently used, according to results from a large clinical trial.
Immunotherapy:
- Emerging Treatments: Research is ongoing into the use of immunotherapy for testicular cancer, aiming to harness the body’s immune system to target cancer cells more effectively.
These advancements are transforming testicular cancer care, leading to more effective and personalized treatment strategies.
