Cancer type > Hematological Cancers
Definition of AUTOLOGOUS TRANSPLANT
An autologous bone marrow transplant (ABMT) is a medical procedure in which a patient’s own bone marrow or stem cells are harvested, stored, and then reintroduced into their body after intensive treatment such as chemotherapy or radiation. This approach is commonly used to treat certain types of cancer and blood disorders. Below is an overview of the procedure, its purpose, and the key steps involved:
An allogeneic bone marrow transplant (alloBMT) is a medical procedure in which a patient receives bone marrow or stem cells from a donor to replace damaged or diseased bone marrow. This approach is commonly used to treat certain cancers, blood disorders, and genetic diseases. Below is an overview of its purpose, process, and key considerations:
Purpose
Cancer Treatment:
Treats diseases like leukemia, lymphoma, and myelodysplastic syndromes.
Immune System Rebuilding:
Used to establish a healthy immune system capable of fighting cancer and infections.
Correction of Genetic Disorders:
Effective for certain inherited diseases like sickle cell anemia or thalassemia.
Treatment of Severe Autoimmune Diseases:
In rare cases, it can help treat refractory autoimmune disorders.
Steps Involved
Donor Selection:
A compatible donor is identified, often a sibling or unrelated individual with a closely matched HLA (human leukocyte antigen) type.
In some cases, mismatched or haploidentical donors may be used.
Stem Cell Collection:
The donor’s stem cells are collected either through bone marrow extraction or peripheral blood stem cell collection after mobilization with growth factors.
Conditioning Therapy:
The patient undergoes high-dose chemotherapy, radiation, or immunosuppressive therapy to eradicate diseased cells and suppress the immune system, creating space for the new stem cells.
Transplantation:
The donor’s stem cells are infused into the patient’s bloodstream via a vein.
These stem cells travel to the bone marrow, where they begin to produce healthy blood cells.
Engraftment and Recovery:
The transplanted stem cells engraft in the bone marrow and start producing new blood cells (usually within 2-4 weeks).
The patient is closely monitored for complications during this phase.
Advantages
Graft-Versus-Tumor Effect:
The new immune system may attack residual cancer cells, reducing relapse risk.
Wide Applicability:
Suitable for treating many cancers and genetic disorders.
Potential for Long-Term Cure:
Provides a complete replacement of diseased bone marrow in curable conditions.
Risks and Complications
Graft-Versus-Host Disease (GVHD):
A condition where the donor’s immune cells attack the recipient’s tissues.
Can range from mild to severe, affecting skin, liver, and gastrointestinal tract.
Infections:
Patients are highly immunocompromised during recovery, making infections a significant risk.
Organ Damage:
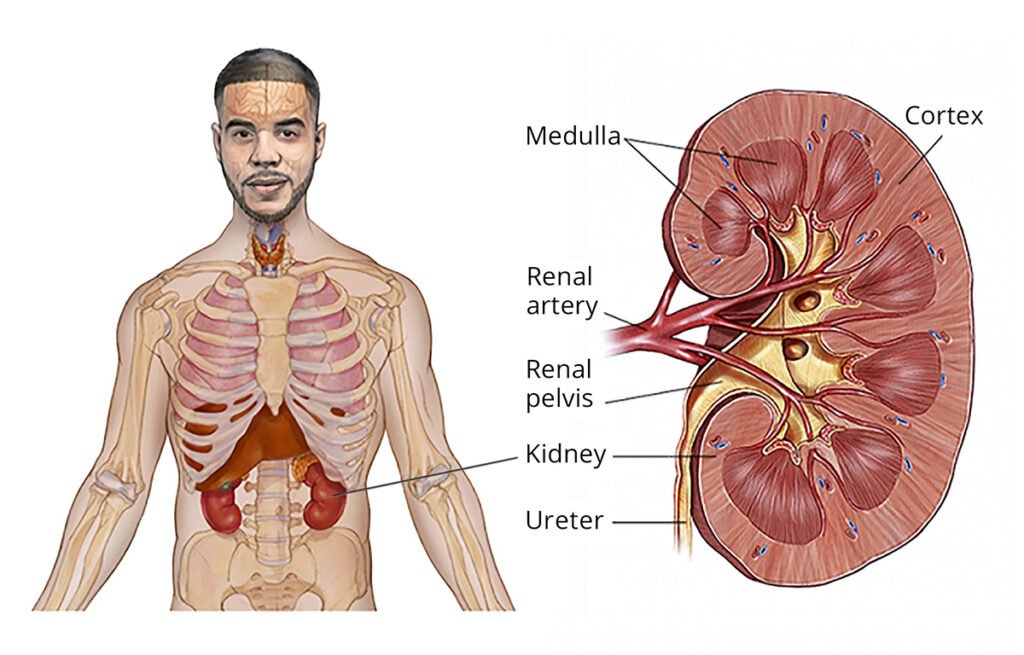
High-dose chemotherapy and radiation can cause long-term damage to organs like the lungs, heart, or kidneys.
Relapse:
The original disease may return, though the risk is lower than with autologous transplants.
Types of Allogeneic Transplants
Matched Sibling Donor (MSD):
The best outcomes are usually with a matched sibling donor.
Matched Unrelated Donor (MUD):
A donor from a registry who matches the patient’s HLA type.
Haploidentical Donor:
A partially matched family member, often a parent or child.
Cord Blood Transplant:
Stem cells collected from umbilical cord blood, used in pediatric or small adult patients.
Indications
Hematologic Cancers: Leukemia, lymphoma, myelodysplastic syndrome, multiple myeloma.
Non-Cancer Disorders: Severe aplastic anemia, sickle cell disease, thalassemia, congenital immunodeficiencies.
If you have further questions about allogeneic bone marrow transplantation or want to understand its suitability for a specific condition, feel free to ask!
AUTOLOGOUS BONE MARROW TRANSPLANT
An autologous bone marrow transplant (ABMT) is a medical procedure in which a patient’s own bone marrow or stem cells are harvested, stored, and then reintroduced into their body after intensive treatment such as chemotherapy or radiation. This approach is commonly used to treat certain types of cancer and blood disorders. Below is an overview of the procedure, its purpose, and the key steps involved:
Purpose
Cancer Treatment: Commonly used for blood cancers like lymphoma, leukemia, or multiple myeloma, as well as some solid tumors.
Recovery from High-Dose Therapy: Enables patients to tolerate high doses of chemotherapy or radiation that would otherwise destroy the bone marrow.
Immune Reconstitution: Helps regenerate a healthy immune system.
Steps Involved
Stem Cell Collection:
Stem cells are collected from the patient’s blood or bone marrow.
In many cases, a process called apheresis is used to collect peripheral blood stem cells after mobilization with growth factors.
Processing and Storage:
The collected stem cells are processed and frozen (cryopreserved) for future use.
Conditioning Therapy:
The patient undergoes high-dose chemotherapy or radiation therapy to eradicate cancer cells and suppress the immune system.
Transplantation:
The thawed stem cells are infused back into the patient’s bloodstream through a vein.
These stem cells migrate to the bone marrow, where they begin to regenerate blood cells.
Recovery Phase:
The bone marrow gradually produces new blood cells (a process called engraftment), which typically takes 2-4 weeks.
Patients are monitored closely for complications such as infection, bleeding, or graft failure.
Advantages
No Risk of Graft-Versus-Host Disease (GVHD): Since the patient receives their own cells, there is no immune rejection.
Reduced Risk of Infection: Eliminates the need for donor compatibility.
Disadvantages and Risks
Infection: The immune system is weakened after conditioning therapy.
Cancer Relapse: Since the patient’s own cells are used, there is a risk that residual cancer cells might be reinfused.
Side Effects: Includes fatigue, nausea, vomiting, and organ damage from high-dose therapies.
Indications
Blood Cancers: Multiple myeloma, non-Hodgkin’s lymphoma, Hodgkin’s lymphoma.
Solid Tumors: Some germ cell tumors.
Non-Malignant Disorders: Rarely, for severe autoimmune diseases or certain hereditary blood disorders.
