Cancer type > Hematological Cancers
Definition of Multiple Myeloma
Multiple Myeloma is a type of cancer that affects plasma cells, a subset of white blood cells responsible for producing antibodies. In this condition, abnormal plasma cells (myeloma cells) accumulate in the bone marrow, disrupting the production of normal blood cells and creating harmful proteins known as monoclonal (M) proteins. These proteins can lead to complications such as weakened bones, kidney dysfunction, and immune system impairment.
Key Features:
Abnormal Plasma Cell Proliferation:
Excessive growth of abnormal plasma cells in the bone marrow.
Bone Lesions:
Bone damage or fractures due to the effect of myeloma cells.
Production of Monoclonal Proteins:
M proteins in the blood or urine, which may cause organ damage.
Symptoms (often summarized as CRAB):
Calcium elevation (hypercalcemia)
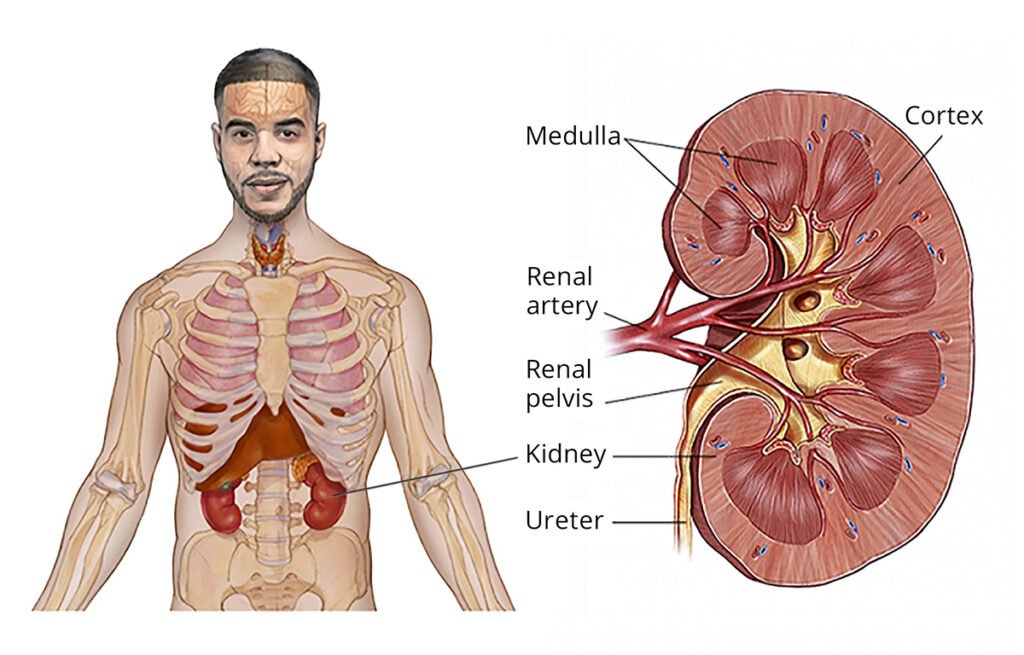
Renal (kidney) dysfunction
Anemia
Bone lesions or bone pain
Diagnosis:
Blood tests (e.g., for M protein levels, calcium levels)
Bone marrow biopsy
Imaging studies (e.g., X-rays, CT, or MRI for bone damage)
Treatment:
Chemotherapy, immunotherapy, targeted therapy
Bone marrow transplant
Supportive care (e.g., for bone health, kidney function)
Multiple myeloma is considered a chronic but treatable condition, with advances in therapies improving survival and quality of life.
SYMPTOMS OF MULTIPLE MYELOMA
Here are the common symptoms of multiple myeloma explained in simple terms:
- Bone Pain: You might feel pain, especially in your back, ribs, or hips. Bones may become weak or even break easily.
- Feeling Tired: You could feel very tired or weak because the disease affects your red blood cells, causing anemia.
- Frequent Infections: Your immune system might not work well, so you could catch infections more often.
- Weakness or Numbness: You might feel weakness or numbness in your legs if the disease affects your nerves or spine.
- Kidney Problems: Your kidneys may not work properly, which can cause swelling in your legs, trouble urinating, or feeling very tired.
- Thirst and Constipation: High calcium levels in your blood can make you feel very thirsty, have dry mouth, or cause constipation.
- Unexplained Weight Loss: You may lose weight without trying.
- Bruising or Bleeding: You might bruise or bleed easily because your blood doesn’t clot as well.
If you have any of these symptoms, it’s important to talk to a doctor, especially if they don’t go away or get worse.
TYPES OF MULTIPLE MYELOMA
Multiple myeloma can be classified into different types based on various factors, including the type of abnormal protein produced by the cancerous plasma cells and the progression of the disease. Here are the main types:
- Smoldering (Asymptomatic) Multiple Myeloma
- Early stage of the disease with no symptoms.
- Abnormal plasma cells and monoclonal proteins (M proteins) are present, but there are no signs of organ damage or symptoms like bone pain or anemia.
- Often monitored without immediate treatment (watchful waiting).
- Active (Symptomatic) Multiple Myeloma
- Characterized by symptoms and signs of organ damage.
- Includes bone damage, anemia, high calcium levels, kidney problems, and infections.
- Requires treatment to manage the disease and prevent further complications.
- Non-Secretory Multiple Myeloma
- A rare type where the myeloma cells do not produce detectable M proteins in the blood or urine.
- Diagnosis relies on other tests, such as imaging and bone marrow biopsy.
- Light Chain Multiple Myeloma
- Produces only parts of the antibodies, called light chains, rather than full antibodies.
- Light chains are detected in the urine (Bence Jones proteins) or blood.
- More likely to cause kidney damage.
- IgG, IgA, IgD, IgE, or IgM Myeloma
- Classified based on the type of immunoglobulin (antibody) the abnormal plasma cells produce.
- Most common types:
- IgG myeloma (most frequent)
- IgA myeloma
- Rarer types:
- IgD, IgE, or IgM myeloma
- Plasma Cell Leukemia (PCL)
- An aggressive and rare form of multiple myeloma.
- Plasma cells are found in high numbers in the bloodstream.
- Requires urgent and intensive treatment.
Each type of multiple myeloma may present differently and require specific treatment approaches.
The exact cause of multiple myeloma is not fully understood, but it involves genetic changes in plasma cells that lead to their abnormal growth and behavior. However, several risk factors are known to increase the likelihood of developing the disease.
Possible Causes
- Genetic Changes:
- Mutations in DNA of plasma cells cause them to grow uncontrollably.
- Changes in chromosomes and oncogenes (genes that regulate cell growth) are often observed in myeloma cells.
- Abnormal Immune Response:
- A history of monoclonal gammopathy of undetermined significance (MGUS), a precursor condition, may develop into multiple myeloma over time.
- Environmental or Occupational Exposure:
- Some chemicals, radiation, or toxins may trigger changes in plasma cells, although the connection is not always direct.
Risk Factors
- Age:
- Most cases occur in people over 60. It is rare in people under 40.
- Gender:
- Men are slightly more likely to develop multiple myeloma than women.
- Race/Ethnicity:
- African Americans have a higher risk compared to other racial groups.
- Family History:
- Having a close relative (parent or sibling) with multiple myeloma or MGUS increases the risk.
- Pre-existing Conditions:
- People with MGUS are at a higher risk.
- Other plasma cell disorders may also increase susceptibility.
- Exposure to Toxins:
- Long-term exposure to certain pesticides, herbicides, or industrial chemicals may increase risk.
- Radiation Exposure:
- High levels of radiation exposure, such as from nuclear accidents, may elevate risk.
- Obesity:
- Being overweight or obese is associated with a higher risk of multiple myeloma.
- Weakened Immune System:
- A compromised immune system, either from illness or medications, may play a role in development.
Key Point
While risk factors can increase the likelihood of multiple myeloma, they do not guarantee that someone will develop the disease. Conversely, people without any known risk factors can still be diagnosed with multiple myeloma.
TREATMENT OF MULTIPLE MYELOMA
Multiple myeloma is a cancer of the plasma cells in your bone marrow. While it can’t usually be cured, there are many treatments to help control the disease, manage symptoms, and improve your quality of life. Your treatment will depend on your age, overall health, and how advanced the cancer is.
What Are the Main Treatments?
- Targeted Therapy
- These are special medicines that attack the cancer cells directly without harming the healthy cells.
- How it works: They block certain proteins that help cancer cells grow.
- Examples:
- Bortezomib (Velcade) and Carfilzomib (Kyprolis) are common targeted drugs.
- Immunotherapy
- This helps your immune system (your body’s defense system) fight the cancer.
- How it works: These treatments help the immune system recognize and destroy cancer cells.
- Examples:
- Daratumumab (Darzalex): A medicine that attaches to the cancer cells so the immune system can destroy them.
- CAR T-cell Therapy: Your immune cells are taken from your blood, modified to attack cancer, and then put back into your body.
- Chemotherapy
- These are strong drugs that kill cancer cells or stop them from growing.
- How it works: Chemotherapy affects fast-growing cells, like cancer cells, but it can also affect healthy cells, causing side effects.
- When used: It’s often given before a stem cell transplant.
- Steroids
- Commonly used medicines like dexamethasone or prednisone.
- How it works: They reduce swelling and kill cancer cells while also helping with symptoms like pain.
- Stem Cell Transplant
- This treatment replaces damaged bone marrow with healthy cells.
- How it works: Doctors collect your own healthy stem cells, give you high-dose chemotherapy to kill cancer cells, and then put your healthy stem cells back into your body to help rebuild your bone marrow.
- Who can get it: It’s often done in younger or healthier patients who can handle the procedure.
- Radiation Therapy
- Uses high-energy X-rays to target specific areas of your body.
- How it works: If cancer has caused pain or damage in certain bones, radiation can shrink the cancer in that area and relieve symptoms.
- Supportive Treatments
- These help manage symptoms and complications caused by multiple myeloma:
- Bone-strengthening medicines like zoledronic acid (Zometa) or pamidronate (Aredia) help prevent bone fractures.
- Pain relief: Doctors may give painkillers or other therapies to ease bone pain.
- Anemia treatment: If you feel very tired, you may need medicines to boost red blood cells or even blood transfusions.
- Kidney care: Medicines and a special diet can protect your kidneys if they’re affected.
- Preventing infections: Antibiotics and vaccines help you avoid getting sick.
- These help manage symptoms and complications caused by multiple myeloma:
How Is Treatment Given?
- Initial Treatment (Induction Therapy)
- The first phase of treatment is designed to reduce the number of cancer cells in your body.
- This often includes a mix of targeted therapy, chemotherapy, immunotherapy, and steroids.
- Stem Cell Transplant or Continuous Treatment
- After the initial treatment, some people may have a stem cell transplant to replace damaged bone marrow.
- If a transplant isn’t an option, treatment continues with medicines to keep the cancer under control.
- Maintenance Therapy
- After the main treatment, doctors may give lower doses of medicines (like lenalidomide) to keep the cancer from coming back.
New and Experimental Treatments
- Bispecific Antibodies: These medicines help the immune system attack cancer cells more efficiently.
- Cancer Vaccines: Research is ongoing to develop vaccines that train your immune system to fight multiple myeloma.
- Clinical trials are testing new medicines, and some of these treatments could be options if standard therapies don’t work.
Lifestyle and Emotional Support
- Healthy Lifestyle: Eating nutritious food, staying active, and drinking enough water can help you feel stronger and reduce side effects.
- Support Groups: Joining a support group or talking to a counselor can help you deal with the emotional challenges of living with cancer.
- Regular Check-ups: You’ll need regular tests to monitor your progress and make sure the treatment is working.
What to Expect
- Many people with multiple myeloma live longer and feel better with today’s treatments.
- The goal is to reduce symptoms, keep the cancer in control, and improve your quality of life.
- Your doctor will work with you to create a treatment plan that fits your needs and goals.
Always discuss your treatment options with your doctor to understand what’s best for you.
PREVENTION OF MULTIPLE MYELOMA
Prevention of Multiple Myeloma
There is no sure way to prevent multiple myeloma because the exact causes of the disease are not fully understood. However, you can take steps to reduce your overall cancer risk and improve your health.
- Address Risk Factors
While some risk factors for multiple myeloma, like age, gender, and family history, cannot be changed, others may be managed:
- Avoid Harmful Chemicals: Minimize exposure to harmful substances like pesticides, herbicides, and industrial chemicals that may increase cancer risk.
- Reduce Radiation Exposure: Limit unnecessary exposure to high levels of radiation.
- Maintain a Healthy Lifestyle
A healthy lifestyle can strengthen your immune system and reduce the risk of cancer in general:
- Eat a Balanced Diet: Include plenty of fruits, vegetables, whole grains, lean protein, and healthy fats.
- Exercise Regularly: Aim for at least 30 minutes of physical activity most days of the week.
- Maintain a Healthy Weight: Being overweight or obese may increase the risk of some cancers, including multiple myeloma.
- Manage Chronic Conditions
Some pre-existing conditions may increase the risk of multiple myeloma:
- Control MGUS (Monoclonal Gammopathy of Undetermined Significance): If you have MGUS, work with your doctor to monitor it closely, as this condition can develop into multiple myeloma.
- Monitor Immune System Health: Avoid activities or habits that weaken the immune system, like smoking or excessive alcohol consumption.
- Avoid Smoking and Limit Alcohol
- Quit Smoking: Smoking can weaken your immune system and increase your risk of many cancers.
- Drink Alcohol in Moderation: Limit alcohol to moderate levels (1 drink per day for women and 2 for men).
- Regular Health Check-Ups
- Monitor Risk Factors: If you have a family history of multiple myeloma or MGUS, regular check-ups can help detect changes early.
- Early Detection: While it may not prevent multiple myeloma, detecting the disease early can improve treatment outcomes.
Stay Informed About Your Health
- Know the Symptoms: Awareness of symptoms like persistent bone pain, fatigue, frequent infections, or unexplained weight loss can help in seeking timely medical advice.
- Seek Medical Advice for Persistent Issues: If you experience symptoms or have risk factors, consult a healthcare professional promptly.
While there is no guaranteed way to prevent multiple myeloma, adopting healthy habits and staying vigilant about your health can help reduce risks and detect issues early.
NEWER ADVANCEMENTS/ RESEARCHES
Recent advancements in multiple myeloma (MM) treatment have significantly improved patient outcomes. These developments include novel therapies and promising clinical trial results.
Bispecific Antibodies
Bispecific antibodies are engineered to bind simultaneously to cancer cells and immune cells, facilitating targeted destruction of myeloma cells. Notable examples include:
- Talquetamab (Talvey): Approved in August 2023, talquetamab targets GPRC5D on myeloma cells and CD3 on T-cells, directing the immune system to attack the cancer.
- Elranatamab (Elrexfio): Also approved in August 2023, elranatamab targets BCMA on myeloma cells and CD3 on T-cells, enhancing immune-mediated cancer cell destruction.
CAR T-Cell Therapies
Chimeric Antigen Receptor (CAR) T-cell therapies involve modifying a patient’s T-cells to target specific proteins on myeloma cells. Recent approvals include:
- Abecma (idecabtagene vicleucel): Initially approved for patients after four or more prior therapies, Abecma received expanded FDA approval in April 2024 for use after two or more prior lines of therapy, allowing earlier intervention.
- Carvykti (ciltacabtagene autoleucel): Approved in 2022, Carvykti has shown promising results in clinical trials, offering a new option for patients with relapsed or refractory MM.
Monoclonal Antibodies
Monoclonal antibodies continue to play a crucial role in MM treatment:
- Sarclisa (isatuximab-irfc): In September 2024, the FDA approved Sarclisa in combination with other treatments for newly diagnosed MM patients ineligible for stem cell transplants, following a study showing a 40% reduction in disease progression or death risk.
Clinical Trial Highlights
Ongoing research is vital for advancing MM treatment:
- CARTITUDE-4 Trial: In June 2024, Legend Biotech announced positive overall survival results from this Phase 3 trial, highlighting the potential of their CAR T-cell therapy in MM treatment.
- Blenrep (belantamab mafodotin): GSK’s Blenrep, previously withdrawn from the U.S. market, demonstrated a nearly 50% reduction in disease progression or death risk in a late-stage trial presented in June 2024, indicating a potential return to the market.
These advancements reflect a dynamic landscape in MM research, offering hope for improved patient outcomes through innovative therapies and clinical trials.
Recent Developments in Multiple Myeloma Treatme
